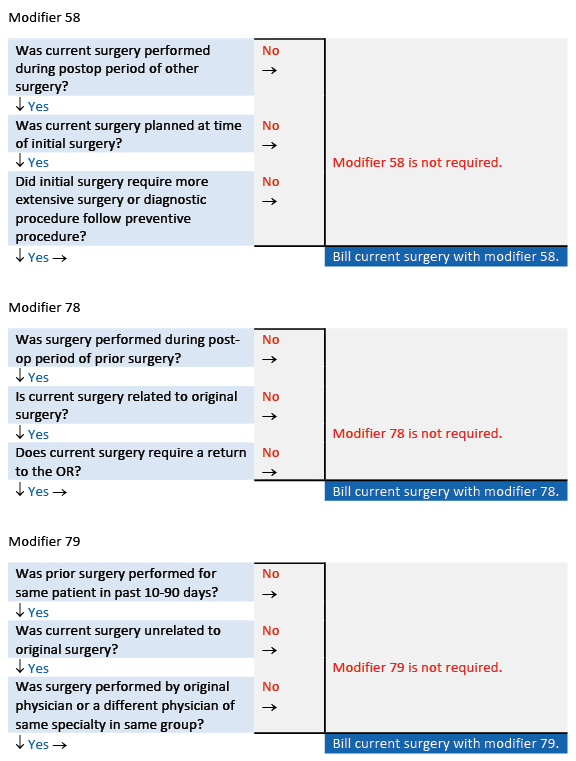
Modifiers 79: Know how to differentiate modifiers 79, 78, and 58to ensure proper reimbursement for all procedures performed.
Modifiers convey important information about a claim and can directly affect reimbursement. But choosing the most appropriate modifier can be confusing — especially when two or more modifiers have similar descriptors. Modifiers 58, 78, and 79 are all used in conjunction with procedures performed within the global period of another procedure and choosing between them can be tricky.
CPT® defines modifiers 58, 78, and 79 as follows:
- Modifier 58 Staged or related procedure or service by the same physician or other qualified health care professional during the postoperative period
- Modifier 78 Unplanned return to the operating/procedure room by the same physician or other qualified health care professional following initial procedure for a related procedure during the postoperative period
- Modifier 79 Unrelated procedure or service by the same physician or other qualified health care professional during the postoperative period
One quick and easy way to distinguish modifiers 58, 78, and 79 is to ask yourself why the physician performed the additional procedure. If it was because of the original condition the initial surgery was treating, odds are you’ll use modifier 58. However, if the reason for the follow-up procedure was because of an unexpected outcome of the prior procedure and not the original condition, modifier 78 may be more appropriate. And in cases where the subsequent procedure was completely unrelated, you may be able to append modifier 79.
If this sounds confusing, it’s because appropriate use of these modifiers is a bit more involved, as we will show you in this article.
Look to Modifier 58 for Anticipated Procedures
Append modifier 58 to the code for the subsequent intervention to indicate the performance of the procedure during the postoperative period was:
- Planned or anticipated (staged) – For example, reconstruction following a major resection. Append modifier 58 for each stage of the reconstruction to ensure the surgeon is paid for the work performed during the global period of the initial surgery.
- More extensive than original procedure – If initial or conservative measures do not achieve the desired outcome as planned, modifier 58 enables the surgeon to be paid when they must go back (during the surgical global period) and do a more radical procedure than was initially performed. For example, a surgeon performs a biopsy, finds cancer, and has to bring the patient back to remove the rest of the tumor.
- For therapy following a diagnostic surgical procedure – For example, the National Correct Coding Initiative Policy Manual for Medicare Services, Chapter 1, General Correct Coding Policies explains, “If a diagnostic endoscopy is the basis for and precedes an open procedure, the diagnostic endoscopy may be reported with modifier 58 appended to the open procedure code. However, the medical record must document the medical reasonableness and necessity for the diagnostic endoscopy.” In this case, open surgery is the therapeutic measure following a diagnostic procedure.
Tip: Do not append modifier 58 for staged procedures when the code descriptor indicates “one or more visits” or “one or more sessions” (e.g., 66762 Iridoplasty by photocoagulation (1 or more sessions) (eg, for improvement of vision, for widening of anterior chamber angle)).
Whether planned or unplanned, in all cases, the follow-up procedure is performed to treat the initial underlying condition, rather than as a result of the prior procedure. The key with using modifier 58 is that it almost always covers a procedure the doctor anticipated before the end of the related, first operation. A new global period begins with each subsequent procedure and, usually, there is no reduction in reimbursement.
Turn to Modifier 78 When Complications Arise
In contrast to modifier 58, which indicates a subsequent procedure that is treating the same condition as the initial procedure, modifier 78 is used for a related operation that was not planned. Specifically, this modifier applies to a situation when the same provider returns to the operating room (OR) during the global period of a previous procedure to treat a problem or condition created by the first surgery.
Simply put, the first procedure results in an unintended outcome that requires the surgeon to bring the patient back to the OR for repair or correction, for example, post-surgical infection, debridement necessitating return to OR, or postoperative hemorrhage. The caveats here are:
- The follow-up procedure must be performed by the same physician or other qualified healthcare professional. Per the Centers for Medicare & Medicaid Services (CMS) guidelines, all physicians of the same specialty in the same group are considered as one when providing services to patients.
- The subsequent procedure must take place in an OR. If the provider is able to treat the complication without a return to the OR, Medicare will bundle the treatment into the initial procedure’s global surgical package.
- The second procedure must be related to the original surgery, not the underlying condition that prompted the first operation. Thus, the diagnosis is usually different for each procedure.
- The use of modifier 78 is not limited to complications. It can be used when the doctor didn’t plan or know of the need for the second procedure until after the first.
For example, a physician removes cataracts from both of a patient’s eyes. Vision in the left eye quickly returns to normal; however, vision in the right eye requires a YAG laser capsulotomy. The second procedure was unplanned, in the postoperative period, and performed by the same surgeon, thus, you may append modifier 78 to the procedure code.
Anytime you append modifier 78 to a code, expect only partial reimbursement, depending on the insurer’s guidelines. This is because codes submitted with modifier 78 typically garner payment for the intra-operative portion of the service only. This amount is typically 70–80 percent of the full fee schedule amount, depending on the presurgical, intraoperative, and postsurgical values assigned to the applicable CPT® code.
Recognize Requirements and the Impact on Reimbursement
Understanding the conditions that determine appropriate use and how each modifier affects payment is important and helpful.
| Modifier 58 | Modifier 78 |
| Breaks the global period and starts a new one. | Does not reset the global period; the global period from the initial surgery remains in effect. |
| Results in full payment. | Results in a payment reduction based on the individual payer’s fee schedule. |
| Subsequent procedure is planned or staged or is more extensive than the initial procedure. | Subsequent procedure is unplanned. |
| Follow-up procedure treats the original problem, not a complication. | Follow-up procedure is performed because of an unexpected outcome created by the initial procedure. |
| Does not require a return to the OR. | Requires a return to the OR or procedure room. |
Differentiate 78 From 79
Append modifier 79 to surgery codes to indicate that an unrelated procedure was performed by the same physician (or a physician of the same specialty in the same surgical group) during the postoperative period of a previous procedure. In other words, look to modifier 79 when the second procedure is not a result of the initial surgery or the diagnosis that prompted it.
Modifier 79, like modifiers 58 and 78, describes a return to the OR by the same doctor during the global period of another procedure; however, modifier 79 indicates that there is no connection between the subsequent procedure and the initial surgery. As such, the unrelated procedure is usually linked to a different diagnosis.
When you append modifier 79 to a code, it starts a new global period. A new postoperative period begins when the unrelated procedure is billed, and the second procedure should be reimbursed at 100 percent of the allowed amount, as determined by the carrier.
CMS defines an OR “as a place of service specifically equipped and staffed for the sole purpose of performing procedures. The term includes a cardiac catheterization suite, a laser suite, and an en-doscopy suite. It does not include a patient’s room, a minor treatment room, a recovery room, or an intensive care unit (unless the patient’s condition was so critical there would be insufficient time for transportation to the OR).”
Reduce Denials, Increase Reimbursement
Discerning when to use modifiers 58, 78, and 79 is understandably difficult, as they seemingly overlap. Just remember: Modifier 58 typically describes “going beyond” the initial intervention — a more extensive procedure, a procedure performed in stages, or providing therapy following a diagnostic procedure — while modifier 78 is for an unanticipated return to the OR to fix a problem created by the first surgery. And when the provider performs two unrelated procedures, with the second being in the global period of the first, append modifier 79 to the second of the two procedures.
Understanding these differences is important, as proper reporting equates to fewer denied claims and higher reimbursement.
For More Information: https://www.aapc.com/blog/65604-append-surgical-modifiers-with-confidence/