In today’s healthcare environment, optimizing revenue cycle management (RCM) is no longer a luxury. It is necessary rising costs, complex regulations and rising patient deductibles are forcing healthcare organizations to spend every penny they can. Fortunately, you can use some effective strategies to streamline your RCM process, reduce errors, and increase profitability. Understanding currency conversion: Before looking at optimization strategies,
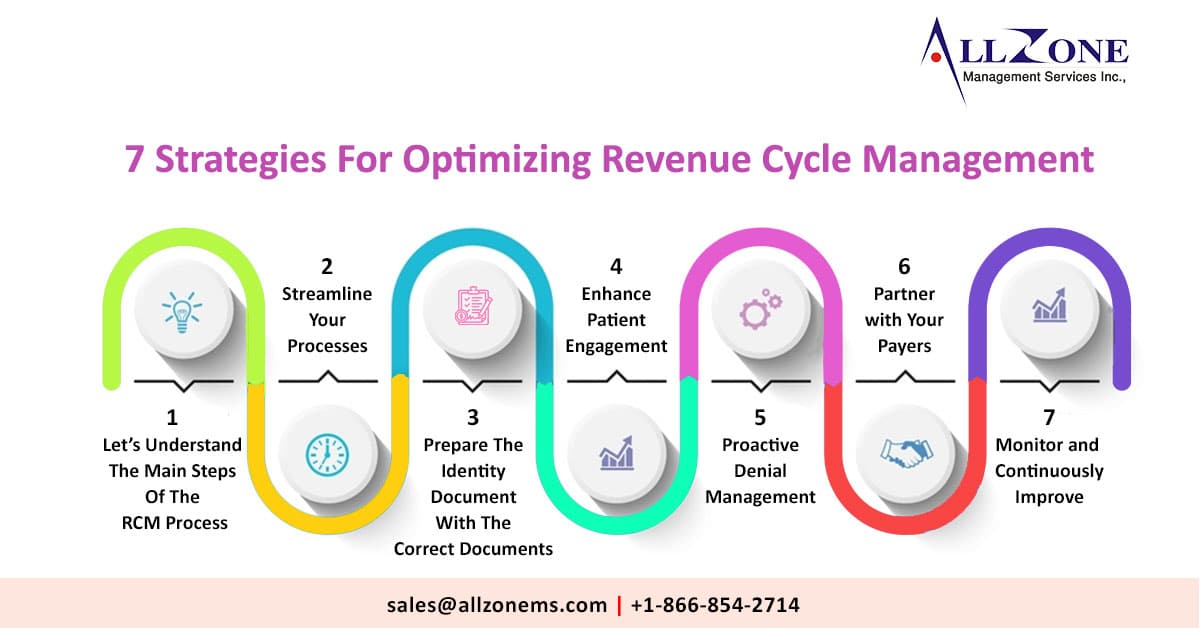
1. Let’s Understand The Main Steps Of The RCM Process:
Registration and Appointment:
Collect patient demographic and insurance information, schedule appointments, and obtain prior authorization as needed.
-
-
- Billing: All billing services provided to patients are properly documented and accounted for.
- Filing a claim: The specified costs are given to the insurance company for payment.\
- Posting Payments: Payments are posted and posted to the accounts payable ledger.
- Denial Management: Denied claims are reviewed and appealed if necessary.
- Patient Collection: We collect balances from patients through various methods.
-
RCM Optimization:
Now that you know your RCM journey, let’s look at some actionable strategies for optimization.
• Technical approval: Invest in new RCM software that automates manual tasks, reduces errors, and improves workflow efficiency. Look for features like:
• Electronic Medical Record (EMR) Integration: Seamless data transfer between clinical and billing systems eliminates duplication and reduces errors.
• Claim Cleanup Tool: This tool identifies and corrects potential errors before a claim is filed, reducing denials and delays.
• Revenue Analytics Dashboard: Get insights into key performance indicators (KPIs) such as days receivable (DAR) and cancellation rates to make data-driven decisions.
2. Streamline Your Processes:
Analyze your current RCM workflow and identify bottlenecks and inefficiencies. Streamline processes, reduce duplication and implement effective communication channels between departments. Think:
• Train transfer workers: This allows workers to fill in during absences and peak periods to keep things running smoothly.
• Use standard templates and forms: Consistent document formatting reduces errors and reduces processing time.
• Automate reminders and notifications: Timely notifications for activities such as claims tracking and patient billing can improve collection rates.
3. Prepare The Identity Document With The Correct Documents:
Medical coding errors are the leading cause of claim denials and lost revenue. Ensure coding staff are properly trained and exposed to coding standards. Apply effective quality control procedures, including regular and quality audits. Add to:
• Streamline documentation: clear and concise notes ensure proper coding and communication with insurance companies.
• Capture all debt services: Don’t waste money missing out on debt payments. Train staff to identify and document all services provided.
• Use coding compliance software: These tools can help you identify and identify potential errors before you submit your claim.
4. Enhance Patient Engagement:
Patients play an important role in the RCM process. By improving communication and transparency, you can increase cost efficiency and reduce administrative burdens. Consider the following strategies:
• Set up a clear and transparent bill: Explain costs and payment options in plain language.
• Offer multiple payment methods: Make it easy for patients to pay online, over the phone, or in person.
• Create a patient portal: Allows patients to access billing information, view information and pay online.
• Train staff to communicate with patients: Equip your staff with the skills to answer questions, resolve concerns and resolve credit issues effectively.
5. Proactive Denial Management:
Don’t wait for the cancellation to happen. Implement a strong objection management strategy that includes:
• Identify denial trends: Analyze data to identify common reasons for denials and focus on preventative measures.
• Supplier Training: Suppliers should be familiar with proper documentation and coding procedures to minimize source disruption.
• Apply the objection early: Don’t let the objection linger. Promptly follow up on denied claims and provide the necessary documentation for appeal.
6. Partner with Your Payers:
Building strong relationships with payers can speed up claims processing, reduce denials, and improve communication. Negotiate with payers, stay on top of policies and negotiate the best rates.
7. Monitor and Continuously Improve:
RCM optimization is an ongoing process. Monitor KPIs regularly, track progress towards goals and identify areas for improvement. We recommend that you perform periodic reviews to identify and resolve compliance issues.
By implementing these strategies, healthcare organizations can optimize their RCM processes, maximize cost, and achieve financial stability.