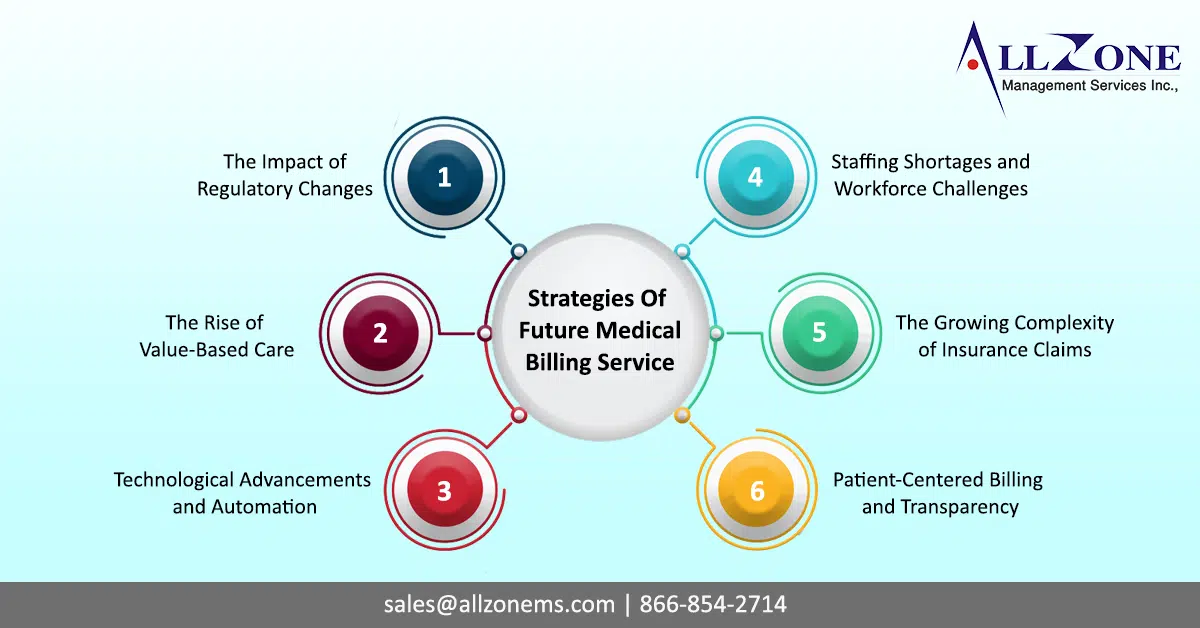
Medical billing is experiencing significant changes as the healthcare industry rapidly evolves. Healthcare providers are facing new challenges managing their revenue cycles as the sector becomes more complex. The future of medical billing services is not without obstacles. However, medical billing services play a critical role in ensuring providers receive timely and accurate reimbursement for services rendered. Medical billing services will need to adapt and innovate to meet several key challenges in the future.
Our newsletter explores the future of medical billing services and discusses strategies to prepare healthcare providers for what’s next.
1. The Impact of Regulatory Changes
Medical billing requirements are continuously evolving. The transition from ICD-10 to ICD-11, the No Surprises Act, and changes in payer policies all require medical billing services to keep up.
ICD-11 Transition
A significant regulatory change has taken place in recent years with the transition from ICD-10 to ICD-11. In addition to offering a more comprehensive classification system suitable for modern healthcare practices, ICD-11 introduces complexities for billing services. For claims to be denied and reimbursed in a timely manner, accurate code usage is essential.
No Surprises Act
Medical billing services have been regulated under the No Surprises Act, which aims to protect patients from surprise medical bills. As a result of this legislation, billing services must work closely with providers and payers to avoid charging patients more than the amount agreed upon for out-of-network services. In order to prevent disputes and ensure compliance, it is essential to provide accurate billing and clear communication.
2. The Rise of Value-Based Care
Health care providers are being reimbursed based on value-based care (VBC). Rather than focusing on the quantity of services provided, VBC rewards providers based on the quality of care they provide, rather than the quantity they deliver. This shift requires medical billing services to adapt by developing new billing processes that are aligned with outcome-based reimbursement.
Tracking Quality Metrics
A value-based care environment requires billing services to collaborate with providers to track and report quality metrics that determine reimbursement levels. This includes ensuring that documentation is accurate, complete, and reflects the care provided. Automation tools that capture these metrics can streamline the process, but billing teams must also be able to interpret the data and apply it to billing codes.
Negotiating with Payers
VBC models will require medical billing services to negotiate new contract terms with payers as they become more common. Billing teams must work closely with providers to ensure that they meet the agreed-upon quality thresholds to maximize reimbursement, which will be more based on patient outcomes than services rendered.
3. Technological Advancements and Automation
Technology is undoubtedly intertwined with the future of medical billing. Despite the potential for improved efficiency and error reduction, these technologies also present a number of challenges that must be addressed as well. Automation and artificial intelligence (AI) are revolutionizing billing processes.
AI and Machine Learning
Automation powered by artificial intelligence can improve many aspects of medical billing, from coding and claims submission to denial management. AI systems are heavily dependent on the quality of the data they are fed. Machine learning algorithms can analyze patterns in denied claims and recommend actions to prevent future rejections. Inaccurate or incomplete data can lead to billing errors, causing claims to be delayed or denied.
Medical billing services must invest in data quality initiatives and train their teams on how to work with AI-based tools in order to fully leverage the potential of AI. Billing professionals can concentrate on more valuable tasks like resolving complex billing issues with these technologies, rather than replacing human expertise.
Robotic Process Automation (RPA)
Another technology that is transforming medical billing is robotic process automation (RPA). The use of RPA can reduce the workload and reduce human error risk by automating repetitive tasks such as data entry, claim submission, and payment posting. In order for RPA to integrate seamlessly with existing billing systems, careful planning is required.
RPA must also be monitored and updated continuously to keep up with new payer rules and billing regulations, as well as ensuring that their staffs are trained to handle RPA workflows.
4. Staffing Shortages and Workforce Challenges
A major challenge facing medical billing is a shortage of skilled workers. The healthcare industry as a whole is experiencing a shortage of skilled workers, and medical billing is no different. The demand for billing services will make it increasingly difficult to find and retain qualified billing professionals.
Remote Work and Outsourcing
Medical billing services have shifted to remote or hybrid work models as a result of the COVID-19 outbreak. Billing companies have been able to tap into a larger talent pool as a result, but it has also created new challenges around workforce management, data security, and team cohesion.
The outsourcing of medical billing services to specialized companies is becoming increasingly popular among healthcare providers facing staff shortages. By outsourcing, providers can access experienced billing professionals without having to manage an in-house billing department. Outsourcing partners must, however, be carefully vetted to ensure they comply with regulatory requirements and provide quality services.
Training and Development
Training and development programs are essential for medical billing services to address staff shortages. Training in new billing codes, regulatory requirements, and technology tools are all part of this program. A billing service’s ability to retain top talent and prepare their teams for the future can be improved by offering career development opportunities.
5. The Growing Complexity of Insurance Claims
Medical billing services must navigate these complexities to ensure claims are submitted accurately and in compliance with payer policies as payers introduce new rules and reimbursement models.
Denial Management
Denial management is a critical component of medical billing, and it is becoming increasingly important as claim denials continue to rise. Several factors contribute to denials, including coding errors, incomplete documentation, and changes in payer policies. In order to identify the root causes of denials and take corrective measures, medical billing services must implement proactive denial management strategies.
Keeping up with changes in payer policy and submitting claims according to the latest guidelines is also crucial for billing teams. While automation tools can help with denial management by flagging potential issues before claims are submitted, human oversight is essential for complex denials to be resolved.
Coordination with Payers
To resolve claims, denials, and reimbursement issues, billing services must maintain open lines of communication with insurers. Effective coordination with payers is essential to successful medical billing. Billing teams must be well-versed in payer policies and have negotiation skills.
6. Patient-Centered Billing and Transparency
The patient’s responsibility for healthcare costs has increased, and billing transparency has become a top priority. Medical billing services must meet patients’ needs for clear, accurate, and timely billing information.
Price Transparency Regulations
Healthcare providers are required to inform patients upfront about the costs of services under recent price transparency regulations. It is essential that medical billing services work closely with providers to ensure pricing information is accurate and reflects insurance coverage. By providing clear, itemized bills to patients, confusion and disputes over unexpected charges can be reduced.
Patient Financial Engagement
Increasingly, medical billing services offer flexible payment options, payment plans, and digital billing options to improve patient financial engagement. Providing patients with tools to manage their healthcare costs and engaging them early in the billing process can help reduce bad debt and improve collections.
Preparing for the Future
The future of medical billing services is marked by both opportunities and challenges. As the healthcare industry evolves, medical billing services must keep pace with regulatory changes, embrace technological advancements, and adapt to new reimbursement models. To thrive in this dynamic environment, billing services must invest in technology, training, and patient engagement.
As well as partnering with experienced billing services, healthcare providers should stay informed about industry trends and adopt strategies to improve their revenue cycles in order to prepare for the future of medical billing services. The healthcare landscape is constantly changing, and providers and billing services need to work together to overcome the challenges ahead.