Prior authorization, the requirement for pre-approval from your insurer for certain services, is a common practice in both Original Medicare and Medicare Advantage (MA) plans. While it helps manage utilization and costs, it can also be frustrating, especially when a request is denied. A 2023 study by health policy research revealed the increasing prevalence of […]
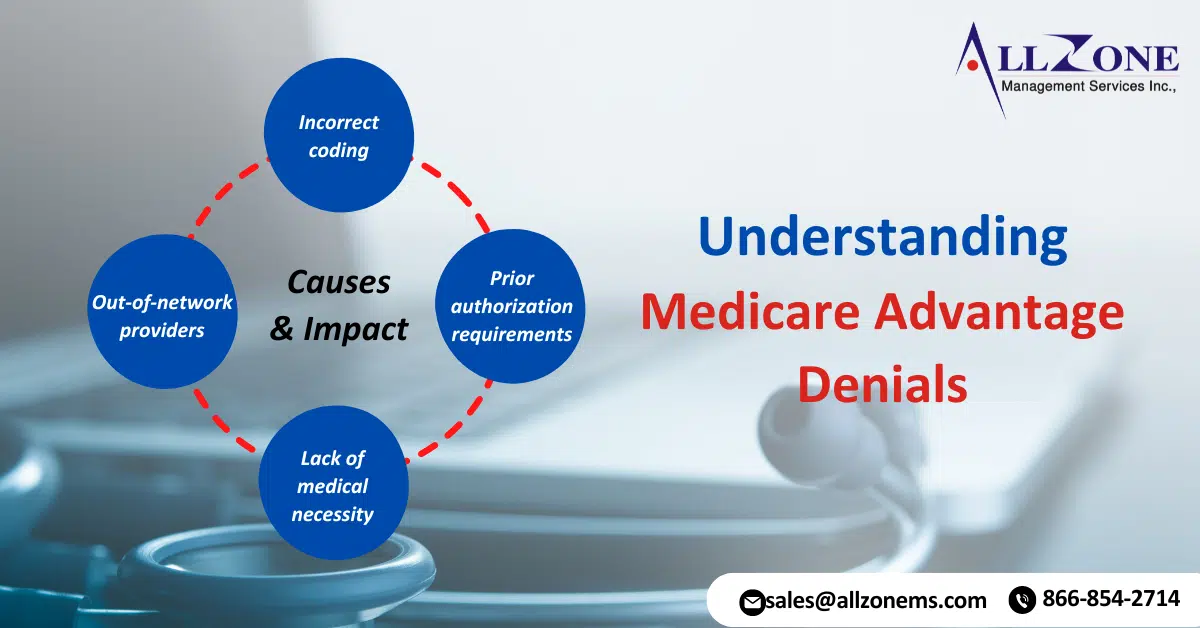
Medicare Advantage (MA) plans, a type of private health insurance, have become increasingly popular among seniors. These plans offer additional benefits beyond traditional Medicare, but they also come with their own set of complexities. One of the most significant issues faced by MA beneficiaries is Medicare Advantage denials for medical services. Recent data has revealed […]
The prior authorization burdens associated with the process have long been a source of frustration for healthcare providers and patients. These burdens can impede optimal care by creating delays in treatment and increasing administrative tasks. However, recent legislative changes and insurer policies aim to alleviate these concerns and streamline the prior authorization process. A radiation […]
Surge in MA Prior Authorization Denials: New Study Reveals A new study highlights significant variation among Medicare Advantage plans regarding the number of determinations made and the frequency of denials. Notably, MA Prior Authorization Denials surged between 2021 and 2022, according to a recent analysis from health policy research. Researchers examined data from the Centers […]
A proposal to track prior authorization using CPT codes was pulled back for revision after a surprising finding. An urologist, advocated for the plan to compensate physicians for time spent on prior authorization requirements. He also hoped it would streamline the process and improve patient care. However, the American Medical Association (AMA) informed urologist that […]
Prior Authorization Challenges are a growing hurdle for medical practices dealing with Medicare Advantage plans. Recent investigations reveal concerning trends: improper denials and a lack of transparency from some insurers. This can significantly delay or even block essential care for patients. The Problem with Prior Authorizations Improper Denials: A government investigation found that Medicare Advantage […]
Streamline Prior authorizations can be a real pain, but with a few adjustments, you can make the process smoother and save yourself and your patients some stress. Here are 5 tips to streamline prior authorizations: Know Your Triggers: Become familiar with medications and procedures that frequently require prior authorization. Identify alternative options, like generics, that […]
Prior Authorization Reform, a lengthy and often frustrating process for payers to control costs, remains a major challenge for doctors. A recent AMA survey of 1,001 physicians found that 89% of physicians believe prior licensure hurts clinical practice. A surprising 33% said the worst things, such as death or hospitalization, were rights-related. The AMA recognized […]
CMS Interoperability and Prior Authorization Final Rule: On January 17, 2024, the Centers for Medicare and Medicaid Services (CMS) published the CMS Interoperability and Prior Authorization final rule (CMS-0057-F). The final rule aims to reduce the burden on patients, providers, and payers by consolidating the authorization process and moving the industry electronically. Affected payers must […]
Getting bogged down by authorization denials? You’re not alone. Here, we explore common roadblocks and effective strategies to keep your revenue flowing smoothly. Challenge: Drowning in Last-Minute Authorizations Solution: Divide and Conquer with a Multi-Team Approach Separate teams can tackle present and future authorizations. The “Today” team verifies benefits and identifies authorization needs for upcoming […]