Outsource RCM: Providers who spend too much on RCM staff and processes, or who experience a high rate of claims denials, should consider outsourcing their medical billing requirements. While our experts chase down payments, you can provide the care, receive the funds, and improve your key performance indicators. Outsource RCM makes sense Why Healthcare Providers […]
Value-based care in 2024: As 2024 approaches, healthcare is undergoing unprecedented innovation and digital transformation. Emerging technologies and capabilities are empowering organizations, including payers, providers, and self-funded employers, to confidently embrace risk within value-based care programs. The American Academy of Family Physicians reports that 49% of practices participate in some form of value-based payment, and […]
Low-dollar accounts receivable for 3 Tips: This can be done effectively, efficiently, and profitably by following the three pillars of low- dollar AR below. Leveraging Offshore Resources for Enhanced Revenue Cycle Management Data doesn’t just tell a story, it can also provide a roadmap for managing low-dollar balances. Use data to identify accounts with the […]
Preventive Services Vs Office Visits: It is important to note that Medicare does not cover preventive services in the same manner as commercial payers. Therefore, it is important to know the patient’s policy and insurance coverage. Table A shows a breakdown of the coverage parameters. Understanding the distinction between Preventive Services Vs Office Visits is […]
NSA Implementation Shortly before Congress adjourns for 2023; lawmakers sent another in a series of letters to the Centers for Medicare and Medicaid Services (CMS) expressing “serious concerns” about the implementation of the No Surprises Act (NSA). The letter accused CMS of failing to properly implement key portions of the law and suggested that the […]
RCM Company has been at the cutting edge of making a difference in healing centers and wellbeing frameworks addressing patient-involved (coordination of benefits) and clinical dissents, recouping on low-balance accounts, and resolving complex claims. Getting these ranges of the income cycle settled rapidly and effectively is becoming tall need these days, as healthcare providers confront […]
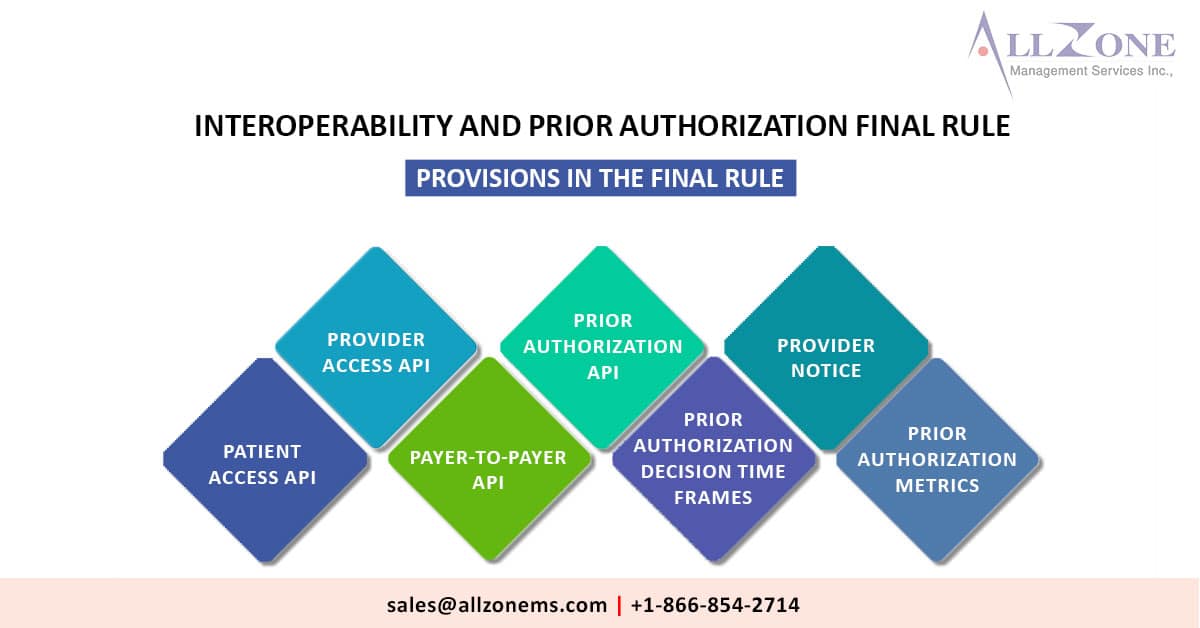
In an effort to streamline prior authorization processes, provider bunches, including the American Medical Association (AMA) and the Medical Group Management Association (MGMA), have asserted that the ultimate goal of the new regulations will assist in facilitating a more efficient and effective prior authorization workflow. Provider bunches are commending CMS for finalizing understanding data-sharing approaches […]
CMS’s Medicaid Payment Model show can be seen as a healthcare bridge, giving fundamental behavioral wellbeing administrations to both Medicaid and Medicare beneficiaries over a period of eight years. As portion of a unused Medicaid Payment Model demonstrate reported by CMS, physical, behavioral, and community suppliers will be required to arrange care in arrange to […]
Affected payers have to be sent earlier authorization choices inside 72 hours for pressing demands and seven days for standard requests. Under a last run the show discharged nowadays, affected payers will be required to send earlier authorization choices inside 72 hours for critical demands and seven calendar days for standard requests. The Centers for […]
The Medicare Advantage and Part D rule was implemented on January 1 by CMS. Despite the fact that the Medicare Advantage and Part D rule which came into effect on January 1, 2019 is now in effect, it is quite early to tell whether 2024 will be the year when providers finally overcome the challenges […]