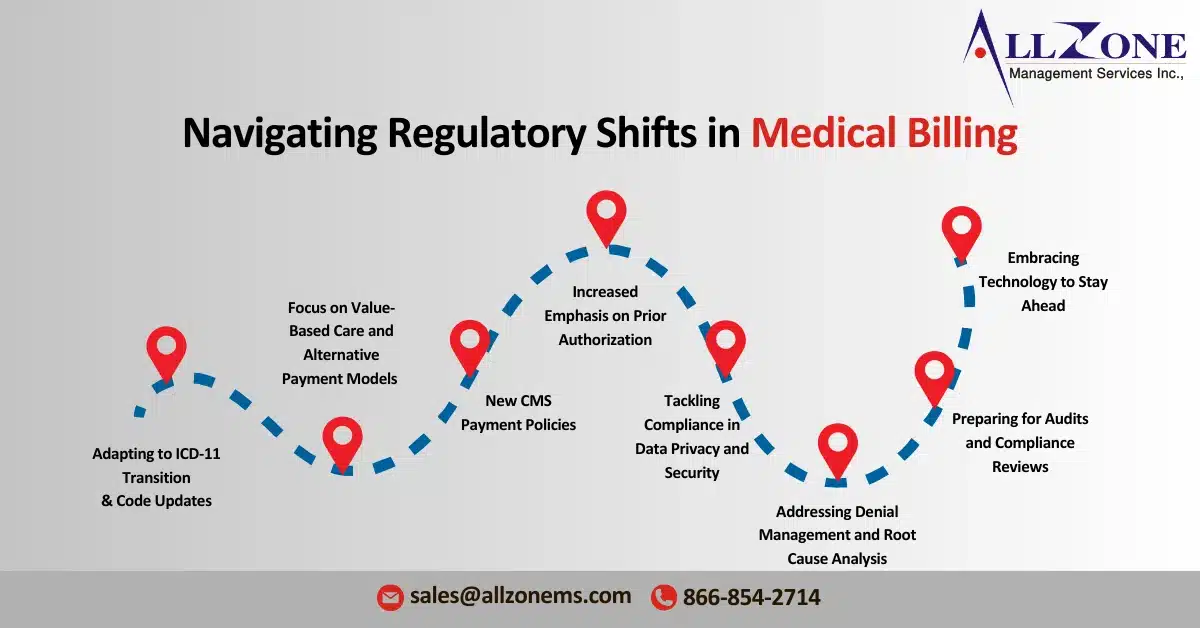
The healthcare landscape continues to evolve rapidly, and 2024 will witness a number of significant healthcare billing regulatory changes that will impact medical billing practices. From updates to code standards to new regulatory compliance requirements, it is crucial for healthcare providers, medical billing companies, and RCM professionals to stay informed and proactive. The goal of this guide is to break down the key regulatory changes that healthcare billing organizations need to address in 2024 and provide strategies for compliance while maintaining efficiency and effectiveness.
Adapting to ICD-11 Transition and Code Updates
One of the biggest challenges in 2024 is the global transition from ICD-10 to ICD-11. As a result of these healthcare billing regulatory changes, although the United States has yet to announce an official date for full adoption, the ICD-11 framework is gaining momentum around the world, which means healthcare organizations must begin to prepare.
Key Aspects of the ICD-11 Transition
-
- Expanded coding categories: ICD11 provides detailed codes, especially for new diseases and new medical technologies. This change allows for more accurate pricing and may result in better pricing if recorded correctly.
- Digital Care: ICD11 was designed for digital platforms, making it easier to integrate with electronic health record (EHR) systems and other billing software.
- Education and training: Staff training is important, as funders, programmers and physicians must be familiar with the structure and applications of ICD-11.
To prepare, medical billing teams can use online resources, attend training sessions, and, if necessary, enter ICD-11 codes to clarify the final transaction.
Navigating New CMS Payment Policies
The Centers for Medicare and Medicaid Services (CMS) is constantly updating its payment policies, and 2024 will be no different. There are several new guidelines related to fee structures and enrollment requirements, particularly for transportation services, telehealth and value-based care practices.
Notable CMS Updates for 2024
-
- Expand telehealth flexibility: CMS has maintained some of the telehealth flexibility that was first introduced during the COVID19 pandemic. This means that providers can offer telehealth services while being billed in many cases based on a personal visit. However, it is important to evaluate which telehealth services are worth the cost.
- Changes to the Medical Facility Payment Schedule (MPFS): The 2024 MPFS includes changes to reimbursement rates, particularly for primary care and mental health services. Businesses need to consider how these rate changes will affect their cash flow and, if necessary, adjust their credit performance.
- Increased Penalties for Noncompliance: Compliance with CMS rules is more important than ever, as the 2024 guidelines introduce greater penalties for errors in billing, documentation and maintenance of patient data.
For compliance, healthcare organizations can establish a dedicated compliance team to monitor CMS updates and incorporate changes into billing and RCM workflows.
Increased Emphasis on Prior Authorization:
Prior authorization will remain a statutory requirement through 2024, with CMS and commercial payers implementing changes to simplify and improve transparency in the prior authorization process. Although the goal is to reduce administrative burdens, healthcare professionals are still struggling to navigate the complex requirements set by different payers.
How to Manage Prior Authorization Challenges
-
- Investing in process automation: Using pre-approval software or automated systems can help track approval status, identify errors and reduce time to get approval.
- Standardization of processes: Standardization helps to reduce errors and speed up the approval process. By creating a unified system, healthcare professionals can manage pre-authorization requests and reduce delays.
- Stay informed about policy changes: Payers often revise their requirements before approval. Checking for these updates regularly will help operations avoid any delays or interruptions.
Training billing teams to stay on top of payer policies and adopting automation can increase pre-approval workflows and improve billing rates.
Focus on Value-Based Care and Alternative Payment Models (APMs)
The shift from fee-for-service (FFS) to value-based care (VBC) continues to shape the regulatory environment. By 2024, more providers will be entering variable payment models (APM) that charge revenue rather than the volume of services provided.
Strategies for Succeeding in Value-Based Care Billing
-
- Implement Quality Tracking Metrics: Accurate documentation of quality measures is essential for compliance and maximizing incentives in APMs. Ensure that the billing team is well-versed in capturing metrics that align with quality-based reimbursements.
- Invest in Data Analytics: Data analytics tools can track patient outcomes, reduce care variability, and identify areas of improvement. These insights not only help in achieving positive outcomes but also boost compliance with value-based reimbursement structures.
- Prioritize Preventive Care and Chronic Care Management: Value-based models reward providers for delivering high-quality preventive and chronic care. Integrating these services into routine billing can ensure practices meet compliance standards and benefit from VBC incentives.
By adapting these strategies, healthcare organizations can successfully navigate regulatory requirements for value-based care and increase patient satisfaction and revenue.
Tackling Compliance in Data Privacy and Security
Patient privacy remains a top priority, with regulatory agencies such as the Office of Human Rights (OCR) enforcing strict guidelines under HIPAA to protect personal health information (PHI). In 2024, as a result of these healthcare billing regulatory changes, regulations will continue to focus on cyber security and privacy.
Best Practices for Ensuring Data Compliance
-
- Regular security audits: Conducting regular audits helps identify vulnerabilities and ensure systems are compliant with HIPAA and HITECH guidelines.
- Data Encryption: Encrypting patient data at all stages of processing and transmission is essential for regulatory compliance and reducing the risk of data breaches.
- Employee training programs: Regular training on cybersecurity and PHI protection helps employees stay aware of emerging threats and reinforces best practices.
As privacy laws become more stringent, healthcare providers must update their systems and processes to prevent unauthorized access and ensure compliance.
Addressing Denial Management and Root Cause Analysis
Denial rates continue to rise due to payer policies, making denial management a vital part of the credit process by 2024. Implementing strategies to prevent, identifying and resolving objections is critical to maintaining cash flows.
Steps for Effective Denial Management
-
- Perform Root Cause Analysis (RCA): RCA is a powerful tool for analyzing recurring objections and preventing them from occurring. By identifying common mistakes and adjusting processes, teams can reduce rejection rates.
- Increase artificial intelligence and automation: Automated systems can identify potential errors before claims are submitted and reduce denials due to incorrect code or missing information.
- Regular staff training: Keeping billing staff informed of changing payer requirements can reduce claim submission errors and improve first-time claim approval rates.
Active objection processing ensures that claims are submitted correctly and, if denied, processed quickly to minimize payment delays.
Preparing for Audits and Compliance Reviews
The 2024 health care sector accounting requirements will be introduced. As a result of these healthcare billing regulatory changes, payers and regulatory agencies are focused on ensuring compliance with accounting and reporting guidelines, which means healthcare providers need to prepare for potential audits.
Audit Preparation Checklist
-
- Maintain accurate and complete documentation: Comprehensive documentation can be a critical factor in audit results. Ensure that records are complete and properly stored for easy access.
- Conduct internal audits: Internal audits always help identify potential problems before external audits are conducted. These audits provide an opportunity to correct errors in documentation or billing practices.
- Create an audit response plan: Prepare a plan that outlines steps to be taken during the audit, including defining responsibilities and establishing clear communication channels.
Through preparation, healthcare organizations can conduct audits with confidence and reduce the risk of penalties.
Embracing Technology to Stay Ahead
One of the most effective ways to adapt in these regulatory changes is to adopt technology solutions designed for credit reporting and compliance. Tools that use artificial intelligence, machine learning and data analysis help organizations adapt to new regulations.
Essential Technology Solutions for 2024
-
- Automated coding tools: These tools can streamline the coding process, reduce manual errors and ensure compliance with new guidelines.
- Revenue management software: RCM software integrates many billing and coding functions, making it easier to track claims, manage objections, and track regulatory changes.
- Data analysis and reporting: Analytics tools provide valuable insights into credit performance, patient outcomes and compliance rates, helping providers make informed decisions and maintain compliance.
Navigating the healthcare billing regulatory changes of 2024 can seem overwhelming, but with the right strategies, tools and teams, healthcare professionals can not only survive these changes, but thrive. By being able to adapt to new codes, payment policies and compliance requirements, medical billing groups can protect their revenue and ensure they are delivering the highest standards of care. As the healthcare industry continues to evolve, it is important to be aware and responsive. A training program, automation and data-driven decision-making can set your organization up for success and make 2024 a year of growth and change.