As 2024 draws to a close, the healthcare industry reflects on a year of groundbreaking innovations, policy shifts, and evolving challenges in medical billing. The Allzone Management Services team has seen first-hand how these changes have improved revenue cycle management (RCM), streamlined processes, and patient satisfaction as a result of these changes. In this newsletter, we delve into critical medical billing insights gleaned from 2024 and discuss the challenges ahead for the industry.
Key Takeaways from 2024
The Rise of AI-Driven Automation
The use of Artificial Intelligence (AI) has continued to revolutionize medical billing in 2024. Automation tools powered by AI have improved claims processing efficiency, reducing human error and administrative workload.
- Predictive Analytics: Predicting claim denials and flagging discrepancies was achieved through the use of AI systems analyzing historical data.
- Natural Language Processing (NLP): Through the use of natural language processing tools, clinical documentation was made more accurate by converting unstructured notes into billable codes.
- End-to-End Automation: Through AI-driven tools, eligibility verification and payment posting were minimized, enabling faster turnaround times and higher reimbursement rates.
Emphasis on Value-Based Care (VBC)
The shift from fee-for-service (FFS) to value-based care accelerated in 2024, driven by policy changes and the growing need to improve patient outcomes. New reimbursement models, such as shared savings programs and bundled payments, presented challenges to providers as a result of this transition. Medical billing teams emphasized the importance of accurate reporting of quality metrics and efficient handling of risk-adjusted coding in order to thrive in this environment.
Regulatory Changes and Compliance
Healthcare organizations faced significant compliance challenges in 2024, including changes to the ICD-10-CM and HCPCS Level II codes. These changes underscored the critical need for accurate medical billing insights to ensure proper documentation and avoid costly audits and denials. Training and upskilling coding teams were critical strategies employed by healthcare organizations to remain compliant and maximize reimbursement.
Focus on Patient-Centric Billing
The increasing financial responsibility of patients for their healthcare led to the need for transparent and user-friendly billing processes. Healthcare providers have implemented the following:
- Upfront Cost Estimations: Preparation of clear cost estimates for patients before services are rendered.
- Flexible Payment Options: A variety of payment options and online portals made it convenient for patients to manage their bills.
- Enhanced Communication: Providing clear, jargon-free billing statements improved patient satisfaction and payment rates.
Tackling Denials with Proactive Management
In 2024, healthcare providers focused on denial management as a top priority. The root causes of denials—from eligibility issues to coding errors—were addressed using data-driven strategies. Providers identified patterns and took corrective action to reduce recurring issues using AI-powered denial tracking systems.
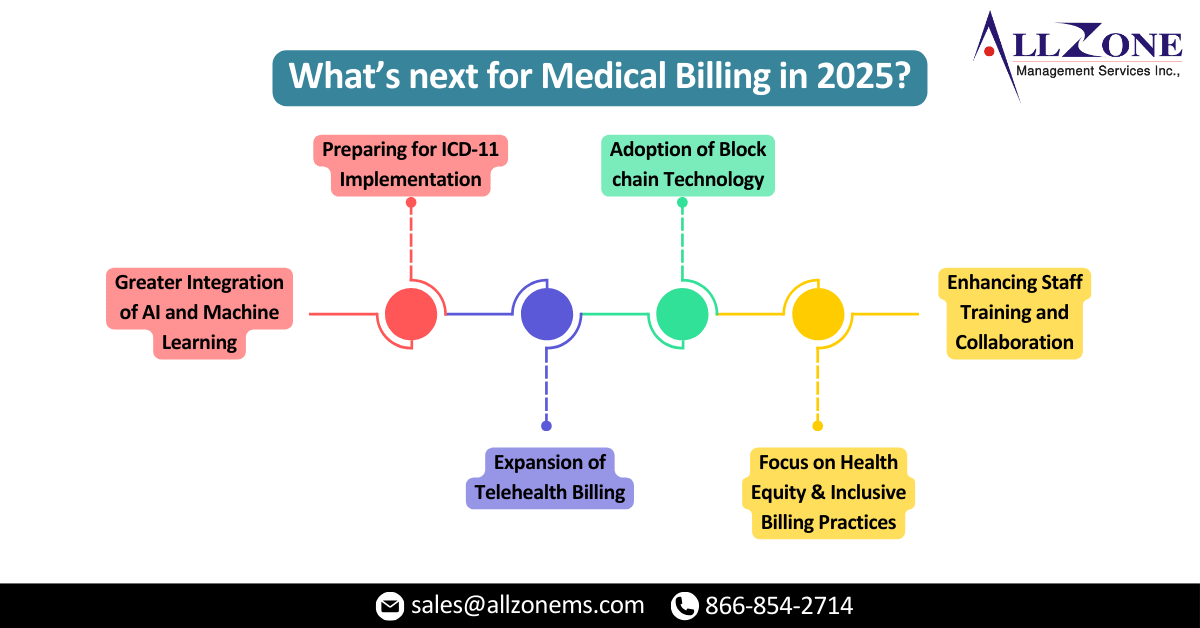
What’s next for Medical Billing in 2025?
Medical billing is poised to grow and evolve in the future, leveraging technology, refining processes, and addressing emerging challenges.
Greater Integration of AI and Machine Learning
AI and machine learning will play an increasingly important role in medical billing processes. Future innovations will likely focus on:
- Real-Time Claims Adjudication: Real-time analysis of payer rules and patient data will enable AI systems to approve claims instantly.
- Enhanced Fraud Detection: The use of machine learning algorithms will reduce instances of fraud and abuse by identifying anomalies in billing patterns.
- Personalized Patient Communication: Patient inquiries will be answered more efficiently by AI-driven Chabot’s, resulting in a more positive billing experience.
Preparing for ICD-11 Implementation
Medical billing teams must prepare for extensive training and system upgrades as ICD-11 is adopted. The transition will bring:
- More Granular Coding: Diagnosis and procedure accuracy are both enhanced by ICD-11, thanks to its increased specificity.
- Global Standardization: Billing services provided by cross-border healthcare providers will be simplified with the new code set, which aligns with international standards.
Expansion of Telehealth Billing
In 2024, telehealth services surged, and this trend is expected to continue. To effectively leverage this growth, healthcare providers must carefully consider the critical medical billing insights related to telehealth. This includes navigating evolving billing guidelines and ensuring compliance with telehealth-specific modifiers like Modifier 95. It will also be crucial for seamless operations to integrate telehealth billing with existing RCM systems
Adoption of Block chain Technology
It is anticipated that in 2025, block chain will be increasingly used in medical billing due to its enhanced data security and transparency.
- Secure Data Exchange: It is anticipated that in 2025, block chain will be increasingly used in medical billing due to its enhanced data security and transparency.
- Smart Contracts: Reimbursements will be streamlined and disputes will be reduced through automated agreements between payers and providers.
Focus on Health Equity and Inclusive Billing Practices
Health equity is increasingly important to healthcare providers, and medical billing practices should reflect this commitment. Disparities will be addressed by:
- Sliding Fee Scales: In order to reach underserved populations, we offer income-based payment options.
- Culturally Competent Communication: Billing support in multiple languages and culturally sensitive payment options are available.
Enhancing Staff Training and Collaboration
It will become increasingly essential for billing teams to invest in education as medical billing becomes more complex. Providers should invest in:
- Advanced Coding Certifications: The latest code sets and billing scenarios are taught through specialized training.
- Interdisciplinary Collaboration: To ensure seamless workflow, clinical, administrative, and billing teams must work together closely.
How Allzone Management Services is leading the Way
Allzone Management Services is committed to staying at the forefront of medical billing innovation. Here’s how we do that:
- AI-Powered Solutions: We streamline every aspect of RCM, from claim submission to payment posting, with our cutting-edge tools.
- Expert Coding Services: In addition to being accurate and compliant with the latest coding guidelines, we have a team of certified coders to assist you.
- Patient-Centric Billing Support: The billing process is transparent and we provide dedicated customer service to enhance the patient experience.
- Training and Consulting: In order to help providers keep up with regulatory changes and emerging trends, we offer customized training programs.
Medical billing must be adaptable and innovative, leveraging the key medical billing insights gained from 2024. In preparing for 2025, Allzone Management Services is committed to providing healthcare providers with the tools and expertise they need to navigate this dynamic environment. We’re paving the way for a more equitable and efficient future in medical billing by embracing technology, encouraging collaboration, and prioritizing patient-centric practices.
To learn more about how Allzone Management Services can transform your medical billing processes, contact us today. Let’s shape the future of healthcare revenue cycle management together.