Denial management in rcm: In the intricate realm of healthcare revenue cycle management (RCM), the substantial challenge revolves around handling denied claims. Scarcity of resources, understaffing, and restricted capacity frequently lead to difficulties in resolving denied claims, where an alarming 82% to 90% are considered potentially preventable. RCM teams can optimize time and revenue recovery […]
According to a survey, claim denials are considered the biggest obstacle in revenue cycle management, with over 20% of providers reporting an annual loss of $500K due to these denials. A recent survey of healthcare leaders conducted by leading medical billing company revealed that claim denials are causing a significant and costly issue for healthcare […]
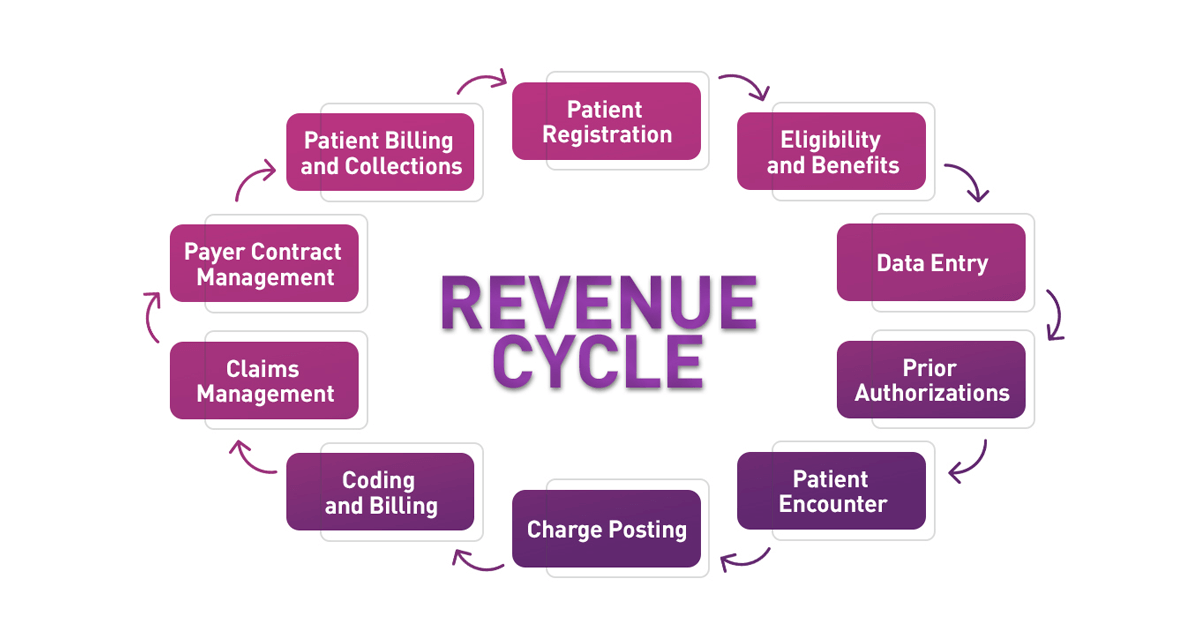
Prompt payment to healthcare providers for their services is crucial for a detailed discussion on managing macro costs, quality, and equity. Without it, addressing the issue of rising healthcare costs becomes challenging. Healthcare providers are well aware that getting paid is not an easy task. A quick search for revenue cycle management (RCM) reveals 16-step […]
Claim scrubbing enables the potential for increased accuracy in claims, enhanced client relationships, and improved patient interactions. Claim scrubbing is the process of identifying and rectifying coding errors in medical claims prior to their submission to insurance providers. Whether conducted manually or through automated systems, claim scrubbers validate medical claims before they are sent to […]
Lately, I’ve been thinking about how to prevent claim denials, especially considering the high number of claims that were denied in 2021. As coders, we can use critical thinking skills to improve the accuracy of our coding and ultimately reduce claim denials. Critical thinking involves formulating questions, gathering information, applying the information, considering the implications, […]
How do you resolve a repeated and shooting up problem like claims denials? It’s been a fresher subject for revenue cycle management professionals for years that are only experiencing hotter with the growing pressures of staffing shortages, troubles with staff movement and instructing and developing policies and protocols at the government and payer levels. On […]
With the arise of indirect health practices such as telehealth, it is becoming increasingly indispensable to play with bill payments and claims orderly. The medical billing cycle is a complex system encompassing procedures such as medical recordkeeping and patient data processing. Medical claim processing is the keystone for healthcare insurance companies since it needs data […]
Denial rates serve as a barometer for the financial well-being of healthcare organizations. An increase in denials can have wide-ranging negative implications for an organization — impacting everything from accounts receivable to the patient experience. By preventing denials upfront, providers can realize revenue faster, boost staff efficiency and satisfaction, and reduce patient anxiety related to […]
Error-free medical billing and coding are critical characteristics of a revamped revenue cycle system. Appropriate billing and coding are not only needed in terms of compliance but are also pivotal in bringing down medical claim denials and rejections. When you take a more dynamic approach to your billing and coding operation, you not only get […]
Medical claims denials are on the rise and continue to be a costly problem for health systems. Unfortunately, the vast majority of providers focus their resources on reactive responses, working to appeal denials and recover payments after denials have already occurred. In a Becker’s Healthcare podcast an expert, discussed the problem of rising denials, why […]