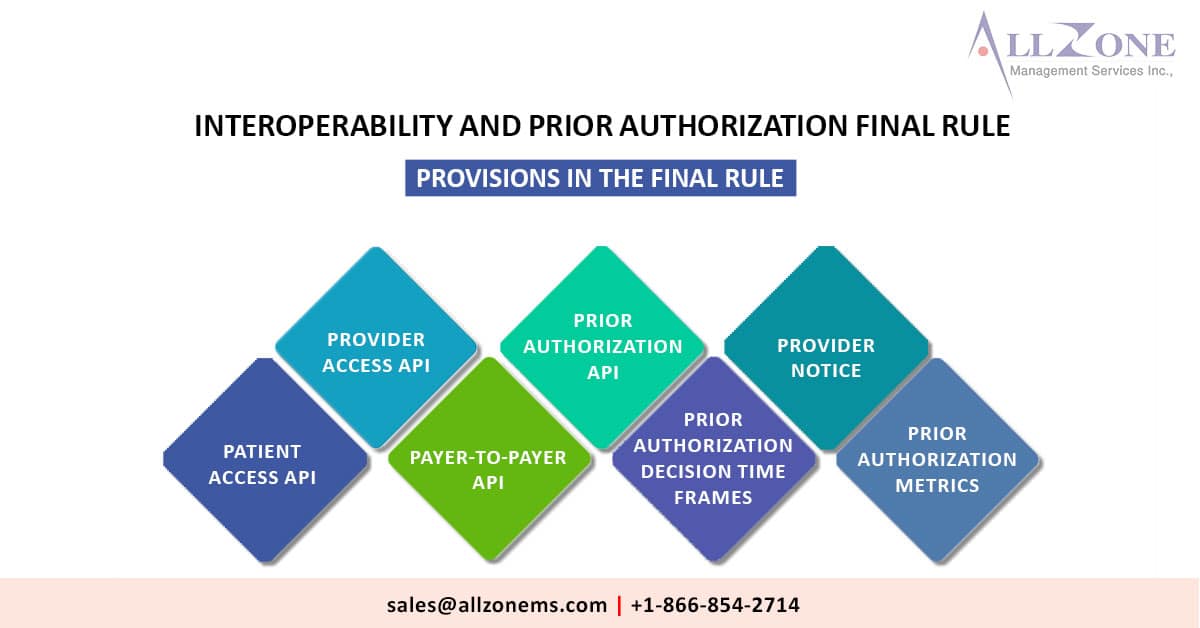
Affected payers have to be sent earlier authorization choices inside 72 hours for pressing demands and seven days for standard requests. Under a last run the show discharged nowadays, affected payers will be required to send earlier authorization choices inside 72 hours for critical demands and seven calendar days for standard requests. The Centers for […]
Tag: Compliance Deadlines in Healthcare
x