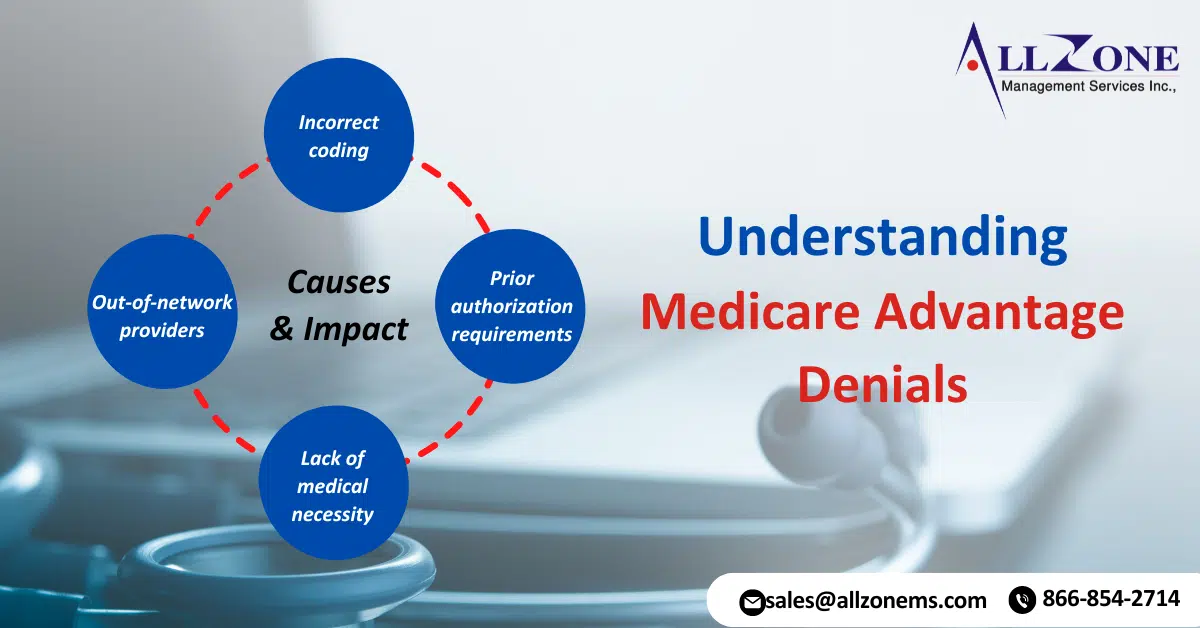
Medicare Advantage (MA) plans, a type of private health insurance, have become increasingly popular among seniors. These plans offer additional benefits beyond traditional Medicare, but they also come with their own set of complexities. One of the most significant issues faced by MA beneficiaries is Medicare Advantage denials for medical services. Recent data has revealed […]
Surge in MA Prior Authorization Denials: New Study Reveals A new study highlights significant variation among Medicare Advantage plans regarding the number of determinations made and the frequency of denials. Notably, MA Prior Authorization Denials surged between 2021 and 2022, according to a recent analysis from health policy research. Researchers examined data from the Centers […]
Cardiology Medical Billing and Coding Process: To effectively handle these changes, cardiology practitioners might have to keep themselves informed about the modifications in payment regulations, modify their billing procedures as needed, and employ novel methods to enhance their compensation. Cardiology billing and coding can be challenging due to various factors, such as the complexity of […]
How do you resolve a repeated and shooting up problem like claims denials? It’s been a fresher subject for revenue cycle management professionals for years that are only experiencing hotter with the growing pressures of staffing shortages, troubles with staff movement and instructing and developing policies and protocols at the government and payer levels. On […]
KEY TAKEAWAYS Denials rose to 11% of all claims last year, up nearly 8% from 2021. Revenue cycle leaders should place their focus on clinical validation denials to help ease the overall denials burden. A key defensive strategy for preventing denials is provider education. Revenue cycle leaders need to understand that clinical validation denials are […]
New patient evaluation and management (E/M) claims are being denied when the patient was previously seen by a specialty physician assistant or specialty nurse practitioner on staff. This is happening when another provider of a different specialty in the same multi-specialty group sees the patient for the first time and bills a new patient E/M […]
Explanation of Medicare Benefits (EOB) error message 96 Non-covered charge was the No. 1 reason for claims denials in December in all of Medicare Jurisdiction H, according to the region’s Medicare Administrative Contractor (MAC). “Prior to performing or billing a service, ensure that the service is covered under Medicare,” Novitas Solutions says on their website. This should be […]