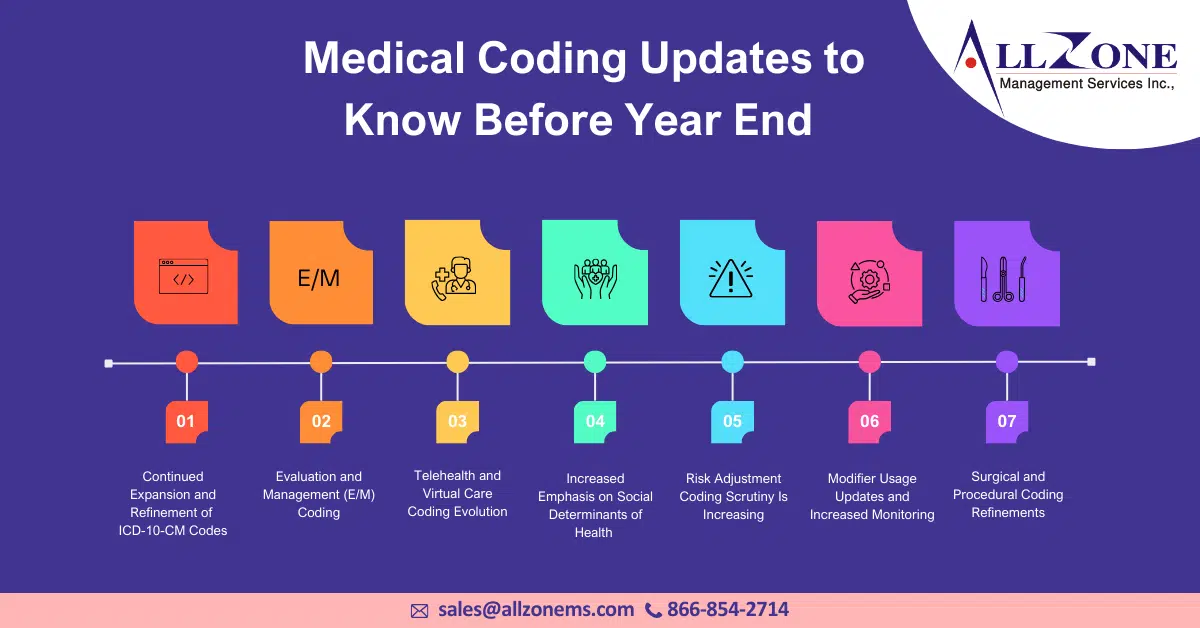
As we approach 2026, the world of medical coding is experiencing a significant shift. This period is arguably one of the most consequential in recent memory. Changes in regulations, the demands of payers, evolving documentation standards, and the increasing influence of technology are all converging to redefine how medical practices handle service reporting, revenue capture, […]
The administrative burden of accurate medical coding is a major contributor to physician burnout—a challenge exacerbated by the COVID-19 pandemic. Studies consistently rank coding-related stress as one of the top concerns for healthcare providers. Medical Coding Mistakes, whether due to oversight or complexity, can have severe financial repercussions for medical practices. Denied claims, reduced reimbursements, […]
Table of Contents Evaluation and Management Surgery: Musculoskeletal System Surgery: Respiratory System Surgery: Cardiovascular System Surgery: Urinary System Surgery: Female Genital System Surgery: Nervous System Radiology Pathology and Laboratory Medicine Category III Codes 2024 CPT Coding updates: Take a look at the updates in CPT coding and guidelines for professional services. Every year, on January […]
The guidelines for interpreting EKGs could vary according to the specific treatment situation. Patients presenting at the emergency department (ED) to undergo an electrocardiogram (EKG or ECG) can present a coding challenge. The main issue revolves around how to accurately report the physician’s services for the patient. Is it appropriate to utilize the EKG CPT® […]
Here are five common mistakes you should avoid to prevent revenue loss 1. Inappropriate medical Coding: Frequently, medical coding for evaluation/management services tends to be excessively aggressive or overly passive, leading to coding errors. These mistakes are primarily due to the misinterpretation of E/M coding guidelines and the fast-paced nature of the clinical environment. Aggressive […]
Providers need a mechanism to be accurately reimbursed for the time and effort that they expend in providing care. Evaluation and Management (E/M) leveling has been the standard method in which to provide appropriate, defensible payments for services. However, it has been successfully argued that the 1995 and 1997 E/M guidelines in place today are […]
Physicians will potentially have a lighter documentation burden and more time to spend with patients in 2021 thanks to an overhaul of Medicare Coding guidelines for outpatient evaluation and management (E/M) services. “The whole point was to have people not document stuff that was not necessary, not relevant to the clinical management of the patient,” […]