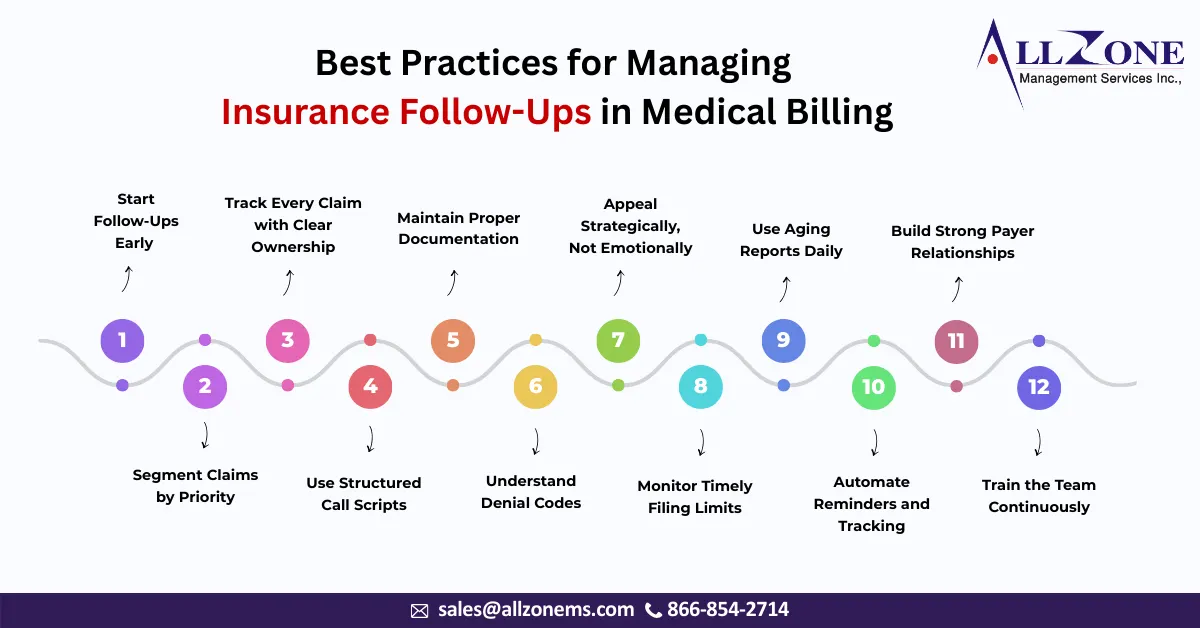
If you ask any experienced revenue cycle manager what truly determines the financial health of a healthcare organization, the answer is rarely coding or charge entry alone. The real difference often lies in one specific operational area — insurance follow-ups. Claims are submitted every day. Payments are expected every day. But revenue is actually realized […]
In essence, the insurance company you billed believes another insurer is primarily responsible for the payment. Understanding and effectively managing CO 22 denial code is critical for maintaining a healthy revenue cycle and ensuring timely reimbursements. This comprehensive guide will break down the CO 22 denial code, explore its common causes, and provide actionable strategies […]
Accounts Receivable (AR) days directly impact cash flow and overall financial health. The longer a claim sits in AR, the more challenging it becomes to collect revenue, leading to cash flow disruptions, operational inefficiencies, and reduced profitability. Therefore, it’s crucial for businesses to actively work to reduce AR days and improve their financial performance. With […]
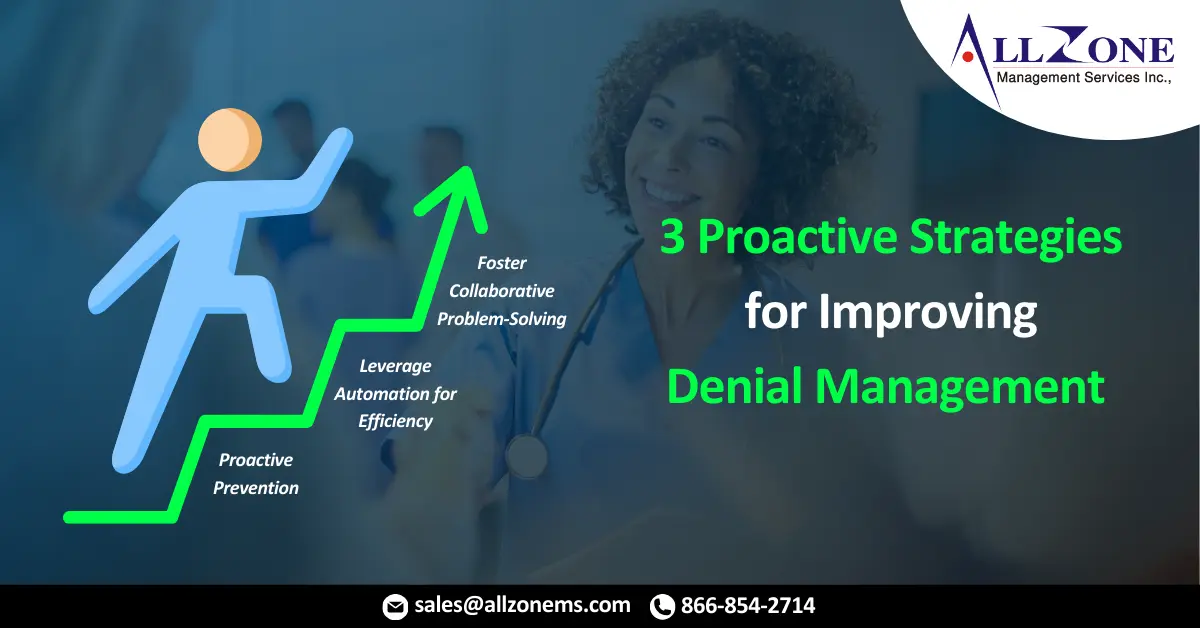
In the ever-evolving field of medical billing, denied claims remain a significant obstacle for healthcare providers. Studies reveal that over 10% of claims face initial rejection by insurers, leading to revenue losses, administrative strain, and frustration for all stakeholders. To mitigate these challenges and ensure financial stability, an effective denial management process is essential. However, […]
During pediatric cardiology internship, witnessed this firsthand. A claim filed nearly a year earlier remained unpaid. The initial denial was due to a missing prior authorization number, a detail buried within the EMR. Unfortunately, the outsourced healthcare billing team took months to decipher this information, causing significant delays in reimbursement. This year-long ordeal highlights the […]
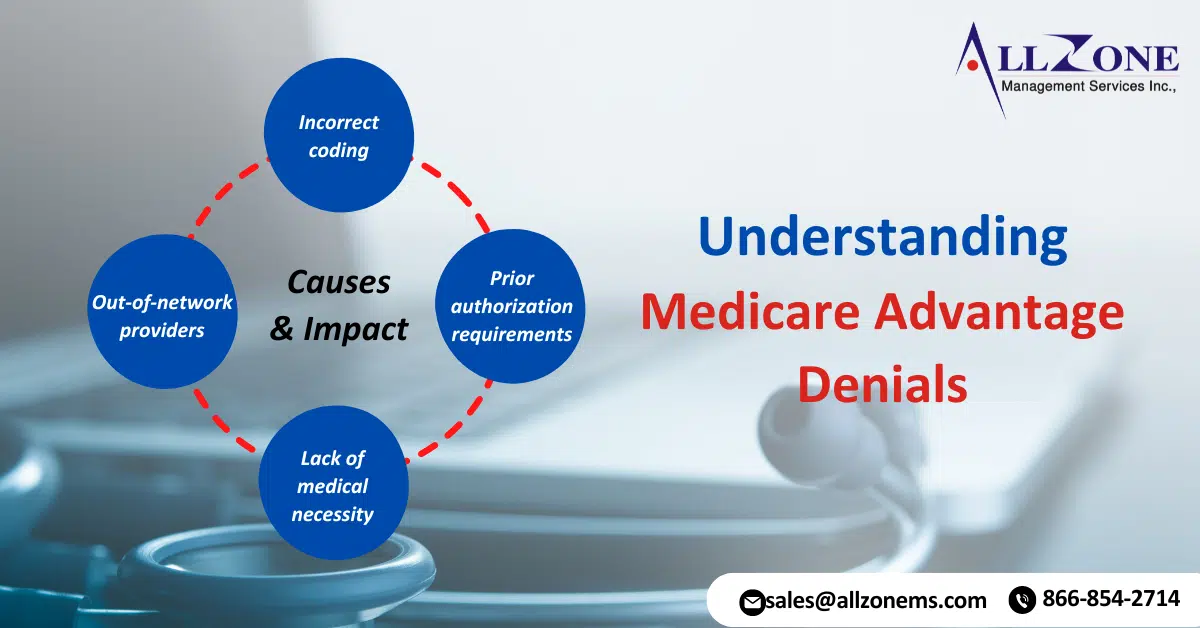
Medicare Advantage (MA) plans, a type of private health insurance, have become increasingly popular among seniors. These plans offer additional benefits beyond traditional Medicare, but they also come with their own set of complexities. One of the most significant issues faced by MA beneficiaries is Medicare Advantage denials for medical services. Recent data has revealed […]
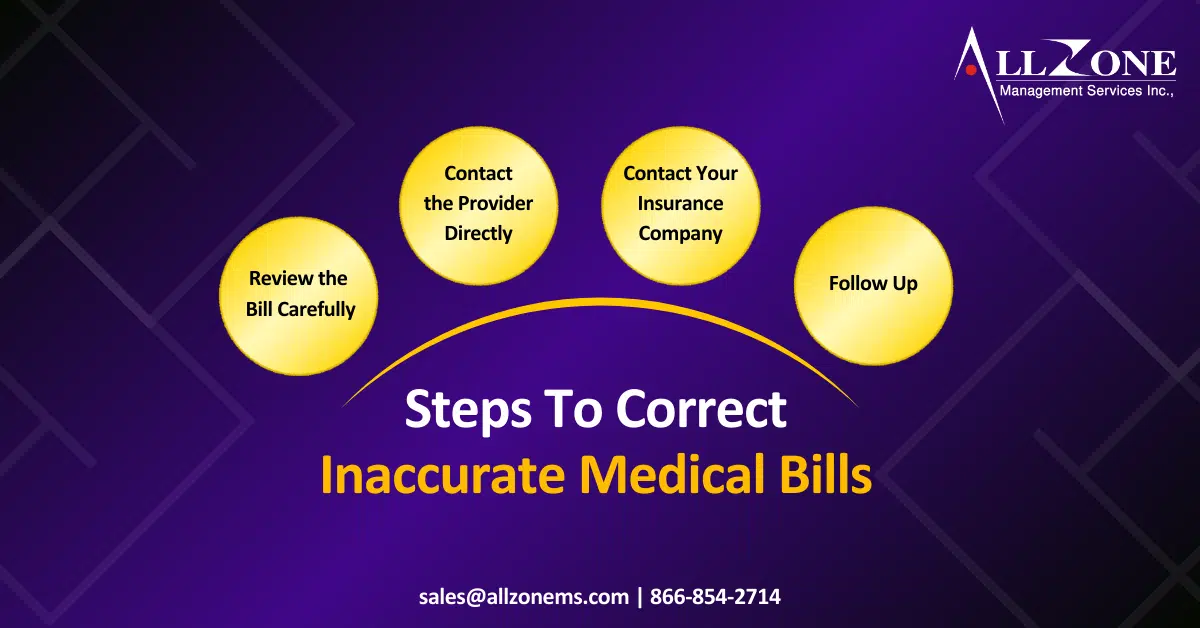
Inaccurate medical bills can be a frustrating and costly experience for patients. From coding errors to duplicate charges, these mistakes can lead to financial strain and unnecessary stress. Understanding the common causes of Medical billing errors and taking proactive steps can help you avoid these issues. Common Causes of Inaccurate Medical Bills 1. Medical Coding […]
Here are some steps to guide you through the process of appealing a denied health insurance claim: 1. Understand the Reason for Denial Review the Denial Letter: Carefully read the denial letter from your insurance company. It should explain why your claim was denied and how you can appeal the decision. Check you’re Policy: Refer […]
As companies shift more and more healthcare costs to their employees, the doormen, office cleaners, cafeteria staff and other members of the union 32BJ SEIU remain among the lucky few who pay no premiums and have no deductibles as part of their benefit plan. Keeping it that way has been no easy task. With each new collective-bargaining agreement, the […]