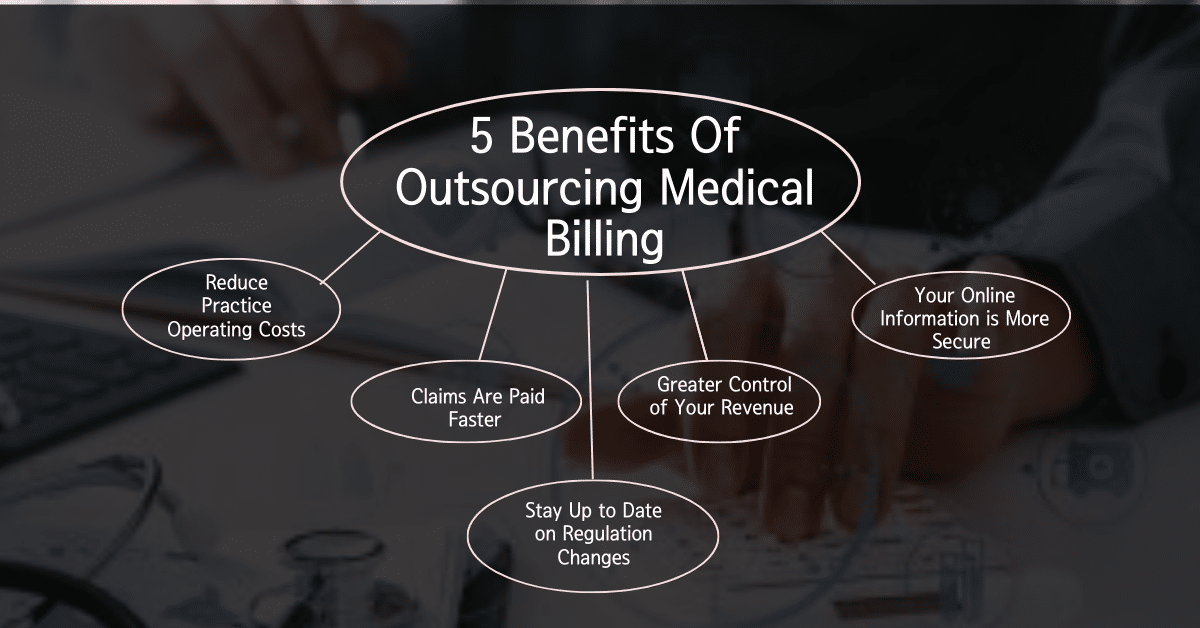
Outsourcing Billing: Hospital and medical professionals acknowledge that the biggest issue they have are receiving payment for their services. Those in the medical field understand all too well the issue of delayed revenue and dormant collections. Though technology has improved the in-office process, the inadequate handling of the hugely important Medical billing process can lead […]
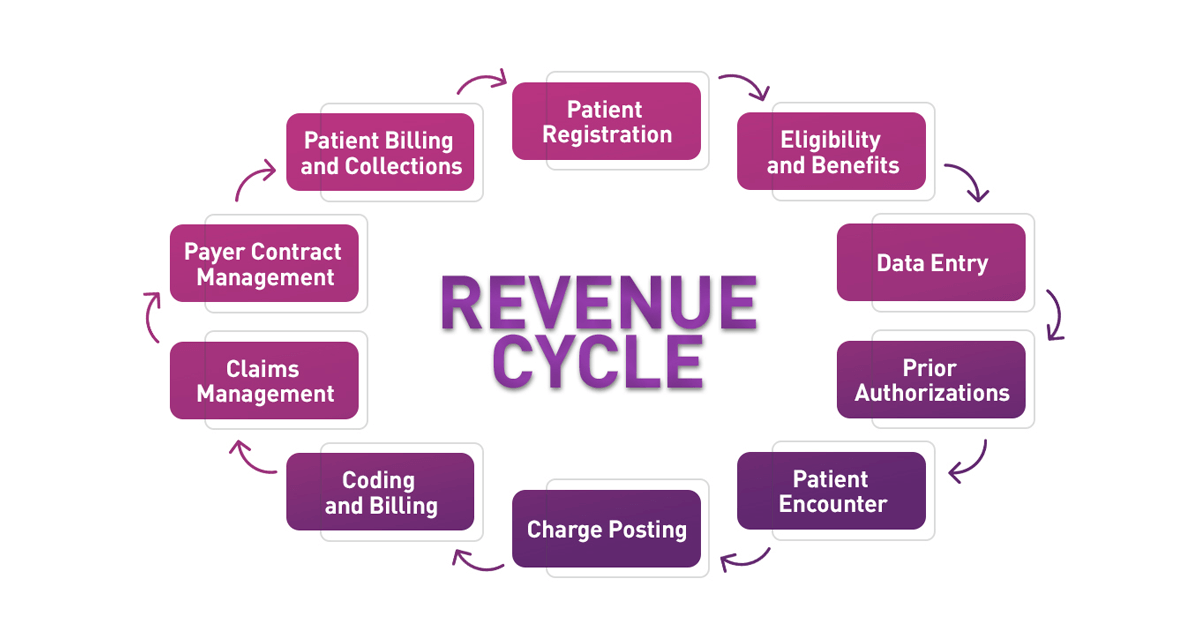
Error-free medical billing and coding are critical characteristics of a revamped revenue cycle system. Appropriate billing and coding are not only needed in terms of compliance but are also pivotal in bringing down medical claim denials and rejections. When you take a more dynamic approach to your billing and coding operation, you not only get […]
Medical claims denials are on the rise and continue to be a costly problem for health systems. Unfortunately, the vast majority of providers focus their resources on reactive responses, working to appeal denials and recover payments after denials have already occurred. In a Becker’s Healthcare podcast an expert, discussed the problem of rising denials, why […]
The billing and collection process in medical offices can be a time-consuming and error-prone process. This can lead to denied claims, uncollected revenue, and frustrated patients. Medical billing companies are looking for ways to optimize this process to improve efficiency, accuracy, and patient satisfaction. One way to optimize the billing and collection process is to […]
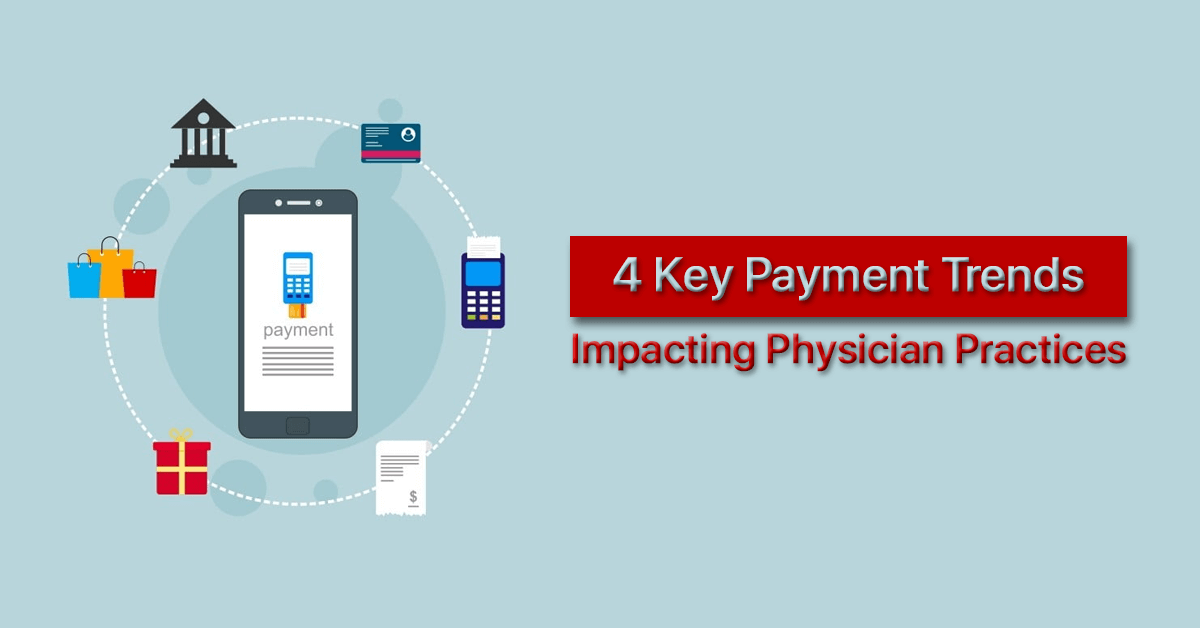
For a modern medical practice, efficiency is everything. Labor costs continue to increase, putting a pinch on practices that are still recovering from pandemic shutdowns. An August 2022 snapshot of practices shows that, although physician productivity is increasing, expenses are growing faster than reimbursements. Every person in the practice must work at peak efficiency, from […]
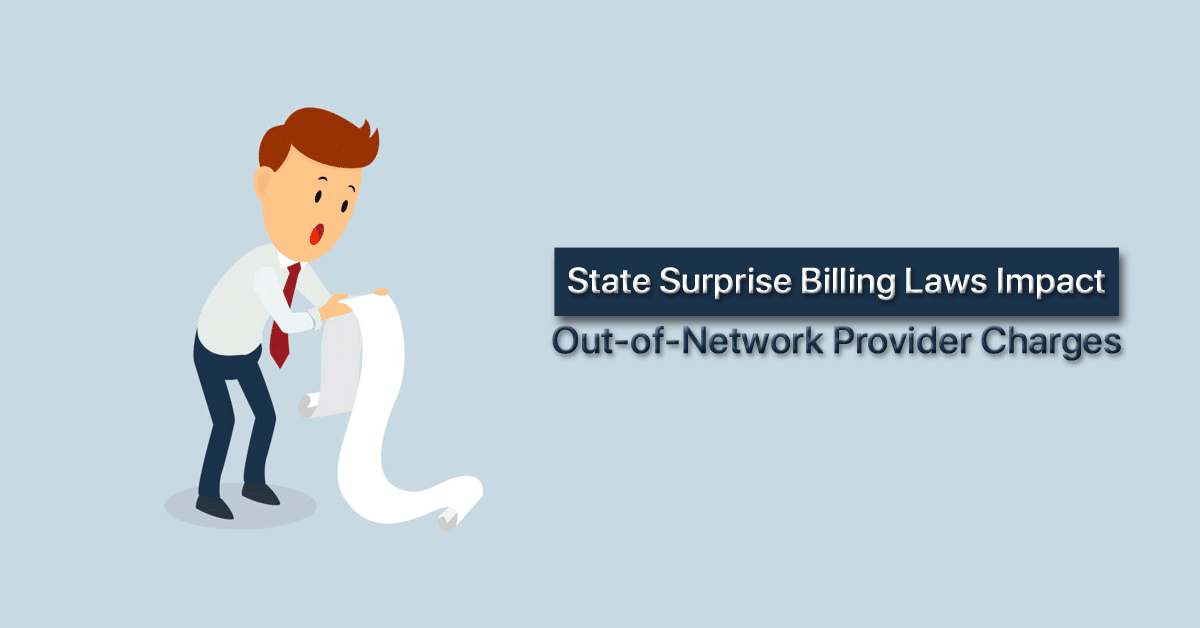
Provider charges for out-of-network care increased by $1,157 after the passage of state surprise billing laws that allow arbitrators to consider provider charges in a surprise billing dispute. State surprise billing laws that allow arbitrators to consider provider charges when determining out-of-network payment amounts for surprise medical bills led to an increase in billed charges […]
The 2023 CPT code set will update the rest of the E/M code section after significant changes in 2021, as well as revise AI and virtual care codes. The American Medical Association (AMA) has released the Current Procedural Terminology (CPT) code set for 2023, which contains updates that aim to reduce medical coding burden for […]
Recent changes to evaluation and management (E/M) billing guidelines that allow physicians to bill for previously unreimbursed services are producing higher revenues for longer patient visits, according to results of a new study. The study in JAMA Network Open looks at the financial impact of CMS’s 2021 expansion of its time-based billing guidelines to include […]
Value-based payment is severely lacking as a percentage of total medical revenue across practices as providers face scheduling and billing challenges. The transition to value-based payment is moving at a snail’s pace despite healthcare’s long journey with the transition away from fee-for-service, new survey data indicates. Value-based payment made up just 6.74 percent of total […]
Failing to post files in a machine-readable format was the most common violation of the hospital price transparency rule among NCI-designated cancer centers. Less than one-third of hospitals with National Cancer Institute (NCI) cancer center designation were fully compliant with the CMS hospital price transparency rule, according to research published in JAMA Surgery. The price […]