Navigating the American healthcare system can feel like traversing a minefield, especially when you’re already vulnerable and seeking treatment. One of the most frustrating and disheartening experiences is dealing with Medical Claim Denials, where a legitimate medical claim is denied by your insurance company. It’s a common problem, and it leaves many wondering: why does […]
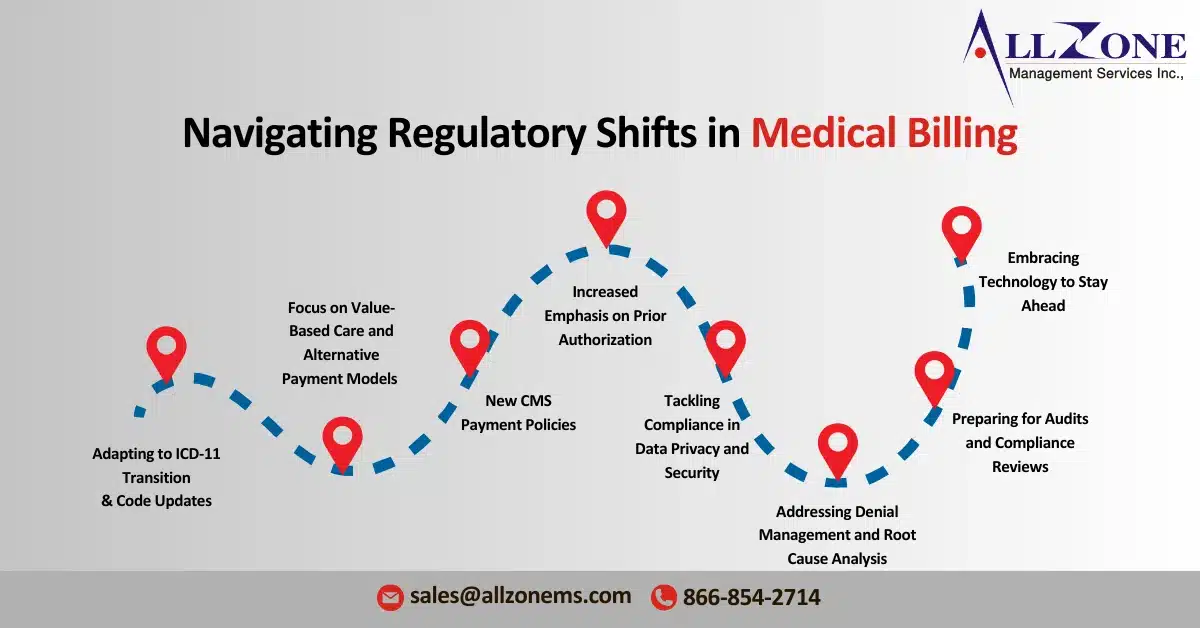
The healthcare landscape continues to evolve rapidly, and 2024 will witness a number of significant healthcare billing regulatory changes that will impact medical billing practices. From updates to code standards to new regulatory compliance requirements, it is crucial for healthcare providers, medical billing companies, and RCM professionals to stay informed and proactive. The goal of […]
Prior Authorization Challenges are a growing hurdle for medical practices dealing with Medicare Advantage plans. Recent investigations reveal concerning trends: improper denials and a lack of transparency from some insurers. This can significantly delay or even block essential care for patients. The Problem with Prior Authorizations Improper Denials: A government investigation found that Medicare Advantage […]
The Medicare Advantage and Part D rule was implemented on January 1 by CMS. Despite the fact that the Medicare Advantage and Part D rule which came into effect on January 1, 2019 is now in effect, it is quite early to tell whether 2024 will be the year when providers finally overcome the challenges […]
Prior authorization still presents challenges to physicians, three years after the AMA and other health organizations released a consensus statement urging reform. A recent survey from the American Medical Association (AMA) evaluated the challenges and roadblocks of prior authorization (PA) for physicians and patients three years after a coalition of industry groups led by […]