During pediatric cardiology internship, witnessed this firsthand. A claim filed nearly a year earlier remained unpaid. The initial denial was due to a missing prior authorization number, a detail buried within the EMR. Unfortunately, the outsourced healthcare billing team took months to decipher this information, causing significant delays in reimbursement. This year-long ordeal highlights the […]
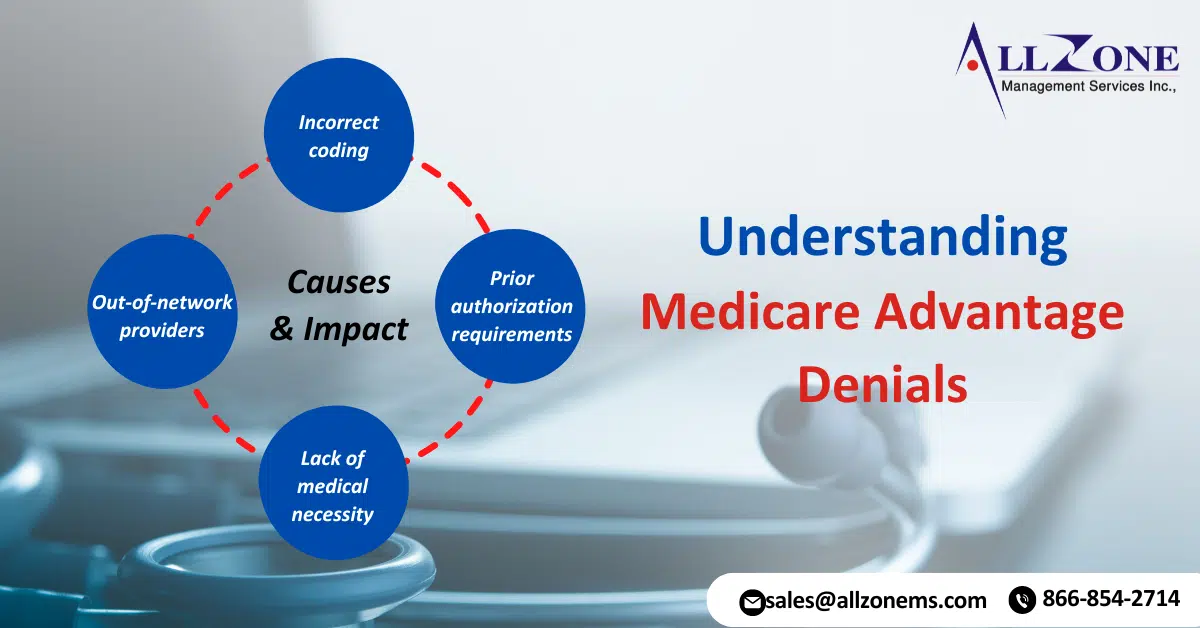
Medicare Advantage (MA) plans, a type of private health insurance, have become increasingly popular among seniors. These plans offer additional benefits beyond traditional Medicare, but they also come with their own set of complexities. One of the most significant issues faced by MA beneficiaries is Medicare Advantage denials for medical services. Recent data has revealed […]
The prior authorization burdens associated with the process have long been a source of frustration for healthcare providers and patients. These burdens can impede optimal care by creating delays in treatment and increasing administrative tasks. However, recent legislative changes and insurer policies aim to alleviate these concerns and streamline the prior authorization process. A radiation […]
Surge in MA Prior Authorization Denials: New Study Reveals A new study highlights significant variation among Medicare Advantage plans regarding the number of determinations made and the frequency of denials. Notably, MA Prior Authorization Denials surged between 2021 and 2022, according to a recent analysis from health policy research. Researchers examined data from the Centers […]
A proposal to track prior authorization using CPT codes was pulled back for revision after a surprising finding. An urologist, advocated for the plan to compensate physicians for time spent on prior authorization requirements. He also hoped it would streamline the process and improve patient care. However, the American Medical Association (AMA) informed urologist that […]
Accurate coding is essential for retina practices performing intravitreal injections, especially when handling retina injection coding. While medication and modifier updates occur frequently, understanding these basics ensures proper reimbursement: CPT® Code Consistency: CPT® code 67028 remains constant for administering the medication. HCPCS Level II Code Tracking: Codes for injected drugs (HCPCS Level II) vary and […]
Prior Authorization Challenges are a growing hurdle for medical practices dealing with Medicare Advantage plans. Recent investigations reveal concerning trends: improper denials and a lack of transparency from some insurers. This can significantly delay or even block essential care for patients. The Problem with Prior Authorizations Improper Denials: A government investigation found that Medicare Advantage […]
The Prime Minister’s recent voluntary national survey shed light on the Denied claims. The survey, conducted between October and December 2023, found that nearly 15% of all Medicare Advantage, Medicaid, Commercial and Managed Medicaid claims were denied. Between 45% and 60% of rejected cases were overturned, although the expensive appeals process sometimes meant multiple appeals. […]
Prior Authorization Reform, a lengthy and often frustrating process for payers to control costs, remains a major challenge for doctors. A recent AMA survey of 1,001 physicians found that 89% of physicians believe prior licensure hurts clinical practice. A surprising 33% said the worst things, such as death or hospitalization, were rights-related. The AMA recognized […]
The Rising Denial Rates in Healthcare Claims Processing Initial Claim Denials: In a new survey conducted by healthcare Company an increased percentage of initial claims are denied by private payers, including pre-approvals for medical claims. Hospitals, health systems, and post-acute care providers may have a difficult time getting paid for medical services. The survey respondents […]